CAR-T Therapy
CAR-T therapy is a personalized immunotherapy used primarily for treating certain types of cancer. Here's how it is created and administered step by step.
Expansion
Genetic Engineering
T-Cell Collection
The engineered T cells are grown and multiplied in large quantities to ensure enough cells are available for treatment.
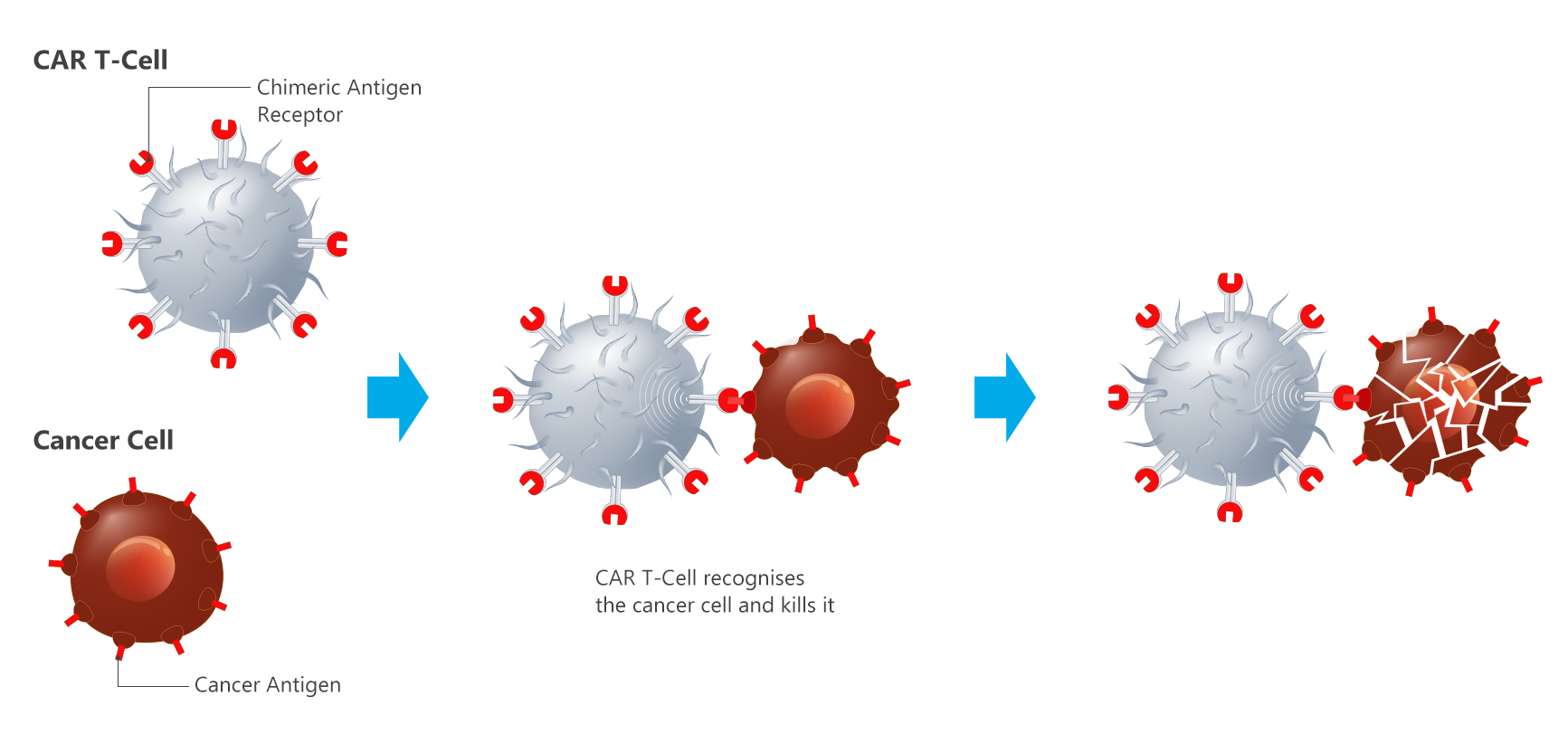
Lab Modification: In the laboratory, the T cells are genetically modified using a viral vector to introduce a gene for a special receptor called a chimeric antigen receptor (CAR).
CAR Function: This receptor enables the T cells to specifically recognize and attack cancer cells by binding to antigens (proteins) on their surface.
Leukapheresis:A patient's T cells (a type of white blood cell critical to immune function) are extracted from their blood using a specialized process.
The collected cells are sent to a laboratory.
Targeting Cancer
Reinfusion
Patient Preparation
Once inside the body, the CAR-T cells recognize and attack cancer cells that express the target antigen.
The engineered T cells can persist in the body for months, providing ongoing surveillance against cancer recurrence.
The CAR-T cells are infused back into the patient through an intravenous (IV) drip.
These cells are now trained to identify and destroy cancer cells with the specific target antigen.
Lymphodepletion: Before the CAR-T cells are infused back into the patient, they may undergo chemotherapy to reduce the number of existing immune cells. This creates space for the CAR-T cells to expand and function effectively.